November is Diabetic Eye Disease Awareness Month: What you should know

Many people know that diabetes can seriously impact a person’s blood pressure, heart health, and stroke risk, but not everyone realizes that the disease is just as dangerous for the eyes.
If you have diabetes, you are more likely to develop glaucoma, cataracts, and diabetic retinopathy.
What is Diabetic Retinopathy?
The inside surface of your eye is lined with a thin, light-sensitive tissue called the retina. Nerve cells in the retina convert light to electrical impulses that are sent to the brain via the optic nerve. It is then translated into images. The nerve cells and tissues in the retina rely on nourishment from tiny blood vessels. In diabetic people, too-high blood sugar levels cause those blood vessels to leak, swell or cease functioning altogether. This condition is known as diabetic retinopathy.
The late stage of diabetic retinopathy causes new blood vessels to grow and leak into the eye’s vitreous fluid. These new vessels may form scar tissue. This leads to a detached retina and ultimately causes partial or complete blindness. That abnormal blood vessel growth is called proliferative diabetic retinopathy and affects about 1 in 20 people living with the condition.
What is Diabetic Macular Edema?
The macula is part of your retina located at the back of your eye and is responsible for your central vision. Macular edema occurs when those swelling blood vessels leak into the macula, causing it to thicken, swell and distort your vision. That may not always lead to blindness or severe vision loss, but it can significantly impact your central vision or ability to see details. Diabetic macular edema is a common problem as diabetic retinopathy progresses.
Are you at risk for Diabetic Eye Disease?
People living with uncontrolled diabetes are at high risk for diabetic eye disease. Other factors that may increase your likelihood of retina damage and vision loss include:
- Long-term diabetes
- Poor management of blood glucose
- Smoking
- High blood pressure and cholesterol
- Pregnancy
- Kidney disease
The only way to diagnose diabetic retinopathy early is through regular eye examinations that search for disease indications in diabetic patients.
Why Diabetic Eye Disease Awareness Month is important
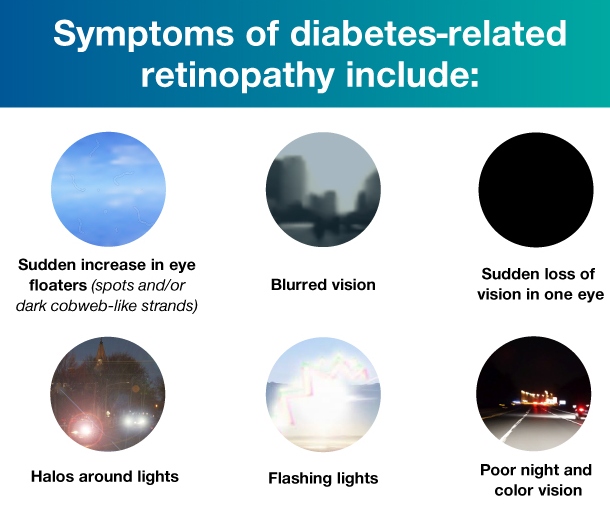
- Diabetic Eye Disease is Scary – Think about all the ways you use your eyes, and now think about how you would feel if you were to gradually lose your eyesight. Diabetic eye disease, also known as diabetic retinopathy, is a group of eye conditions affecting people with diabetes. These conditions include cataracts (clouding of the eye’s lens), glaucoma (elevated pressure inside the eye), and macular swelling (optic nerve damage). If you have blurry or frequently changing vision, experience dark areas or vision loss, or if you see “floaters” or flashes of light, consult your optometrist immediately.
- All types of diabetes can trigger eye disease – It’s just a fact that if you suffer from diabetes, you have a greater chance of having an eye disease than someone who doesn’t. Every type of diabetes makes you vulnerable, which is why early detection with regular eye exams is key. People with types 1 and 2 diabetes need annual exams. Pregnant women with both types 1 and 2 need exams prior to pregnancy or at least during the first trimester.
- Prevention means dilating your eyes – If you have diabetes, you need a more in-depth exam where the eye doctor dilates your eyes. This means you will receive drops in your eyes to make the pupils larger. This allows the optometrist to fully see the back of each eye including the retina, blood vessels, and optic nerve. After your eyes are dilated, don’t panic if your vision is slightly blurry for a couple of hours — but make sure to arrange for transportation.
CONTACT US NOW TO BOOK YOUR APPOINTMENT!
